Early Clinical Investigators
Being involved in clinical trials as a new Principal Investigator (PI) may present unique challenges for the early investigator faculty. This is because curricula and practical experience with clinical trials during fellowship training are often limited. For example, while pediatric rheumatology fellows and med-peds adult rheumatology fellows may be involved in clinical drug trials during fellowship, the extent of their involvement is often limited to identifying patients for study enrollment. Fellows may be involved in completing study visits which includes seeing patients and filling out case report forms. However, fellows are not typically the Principal Investigator (PI) on clinical trials. As such, fellows are not exposed to the process of verifying eligibility of their site and/or enrolling their site for clinical trials. Exposure to the “business” side of trials such as budgeting and contracting processes with pharmaceutical companies and other related entities is often lacking.
The PORTICO Clinical Trials toolkit is a curated series of publicly accessible videos and links covering essential operational details that early investigators need to know before embarking on a clinical trial with a special focus on pediatric trials.
Clinical Trials Toolkit — PORTICO (porticocenter.org)
Frequently Asked Questions you might have are addressed below. A short overview of FAQs is listed in the first tab, while more detailed explanations are provided in the tabs below.
- What are some key responsibilities for Principal Investigators (PI) when involved in industry sponsored studies?
- A PI oversees and is responsible for the execution of the clinical trial at their site.
- A PI must ensure protection of the rights, safety, and welfare of all study subjects.
- How do I estimate the number of patients that can be enrolled and why is this important?
- You can run an ICD-10 query or use SNOMED-CT (Systemized Nomenclature of Medicine-Clinical Terms)
- As a PI you need to estimate the number of subjects you think is feasible to contribute to the study a priori.
- What are some key determinants of costs in an industry sponsored study – what needs to be in the site budget?

- What role do CRO’s play in industry sponsored studies?
- CRO’s, or Contract Research Organizations, must ensure that the clinical sites are following the protocol and that the trial is being conducted in compliance with regulatory requirements and ethical principles.
- Who prepares the contract and budget for industry sponsored studies?
- The Legal team at your institution prepares the contract.
- The Research Department prepares the budget.
- What are some key time-consuming activities to consider when taking part in an industry sponsored trial?
- Time to IRB approval.
- Time for legal teams to develop and negotiate the contract.
- Time for budget negotiations.
- How long should I expect to wait between site selection and initiation of screening?
- This varies from site to site and between different pharmaceutical companies
- Average time to complete IRB approval, budget and contract should take between 3-6 months
- What is the difference between a Local IRB and Central IRB, and which should I choose if given the choice?
- A local IRB is your hospital’s IRB.
- A central IRB is an IRB that conducts reviews on behalf of all study sites.
- In most cases, choosing to rely on a central IRB will improve efficiency and reduce costs.
- What are some considerations when deciding to participate in a non-PRCSG industry study?
- Protocol may not be pediatric friendly (e.g., no free drug after the trial completes).
- Lack of publishing opportunity.
What are some general PI Responsibilities?
The PI engages in completing the feasibility questionnaire for a study, taking part in the industry pre-study site visit, and ultimately deciding whether to conduct the trial at their center. Once the trial is underway, the PI is responsible for enrolling subjects, making sure the study is conducted as per protocol, signing off on adverse events reports, responding to queries, signing eCRF forms, and taking part in monitoring site visits. As a site PI you will be asked to complete FDA form 1572, which is a signed agreement to comply with FDA regulations during the conduct of the clinical investigation of a drug.
How is the PI involved in the Budget determinations?
The role of the PI is not to go back and forth in contract negotiations over legal language- let your hospital’s legal team do this. Site PIs also should not directly negotiate with industry about the budget- let your hospital’s budget team, which typically resides in the research department, deal with this. However, the PI needs to be aware in broad strokes of what is being decided with the contract and budget, especially when there are disputes over language between the drug company (Sponsor) and your institution.
Keep in mind that both the legal and budget teams can take quite a while to make decisions. Negotiations typically happen over several weeks to several months. This can and will slow down your ability to be able to recruit to the study and needs to be considered when projecting salary allocations for your study team. You will need to have your CRC stay on top of this process as much as possible (e.g., CRC updates PI in weekly meetings) and intervene with your team if discussions get “stuck”.
When approached for being an investigative site one of the first questions you will be asked is, “How many patients can be enrolled at your Center?”
How can you determine the amount of patients you can enroll?
There are a couple of ways to determine the number of patients you have with a certain diagnosis. First, you can see how many patients have visits assigned relevant ICD-10-CM codes during the coding and billing process. The downside of this approach is the dependence on how accurately providers enter ICD-10 codes. Requiring more than one visit with the relevant code or restricting codes to those assigned by your rheumatology department/division can help increase the likelihood that the patients actually have the diagnosis. Another option is to use SNOMED-CT, which may be available in your institution.
What are the consequences of an overestimate?
Some Centers lack processes to accurately estimate how many patients are actively followed. Thus, the PI or CRC must guess how many patients have the condition being studied when filling out the feasibility questionnaire for the study. This may lead to overestimating the number of subjects that can be recruited. If a high estimate is given and then only a few patients are enrolled, the Contract Research Organization (CRO) will be asking you constantly to enroll more subjects, which isn’t possible because you don’t have the volume.
What if you are unable to enroll a large sample size?
The number of subjects you will enroll in clinical drug trials is typically low, which is risky since there is a chance you will not enroll any patients. Failure to enroll will leave you with a deficit at the end of the trial since part of the revenue you anticipate generating depends on actual enrollment in the trial. In PRCSG’s opinion, enrolling one subject will lead to breaking even. Thus, be conservative in your estimates as you also cannot assume that any suitable patient wants to be part of the study.
How long should we expect the Drug Study Timeline to be?
You will want your CRC or research department to produce a schematic on an Excel spreadsheet so you can understand how long each task should take and identify where in the process things are. Examples of items to include in the timeline include the following: Signing of the Confidential Disclosure Agreement or Non-Disclosure Agreement (CDA or NDA), completing a feasibility questionnaire, pre-study visit (PSV), site selection visit (SSV), site qualification visit (SQV), protocol and study package review, contract and budget negotiation, Institutional Review Board (IRB) submission, and the start-up visit. Time to completion of these various timelines varies, but in general IRB submission, contract and budget should not take more than 6 months.
Major Budget Considerations:
The main focus tends to be cost per patient, which is multifactorial and includes how many subjects you will enroll and how much money the center receives per patient. Next, one needs to determine the payment to subjects per visit as a means of compensating the subjects for their time in the trial.
Additional Budget Considerations:
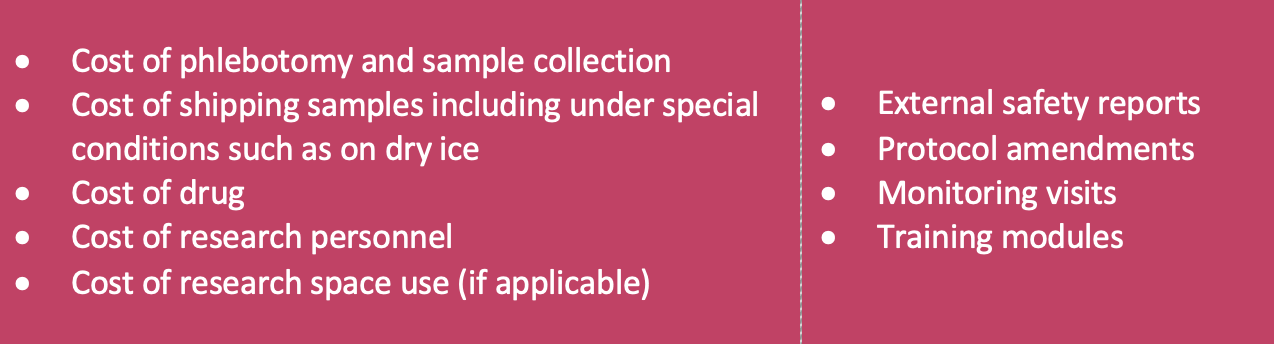
The cost of the 4 items in the right cell on the table above are often underestimated and this can lead to a study deficit at the end of the study. To avoid this, include a budget item for “yearly administrative fees” that accounts for all these items (e.g., in 2024 a large Children’s Hospital asked for $15,000 to $20,000 in administrative fees).
What if you need to change the budget later on?
Keep in mind you can re-negotiate these ancillary study costs during the study. For example, prior to the study, you estimate in the budget that there will be 5 monitoring visits to your site. 3 months after the study began, there have already been 5 visits and there are 12 months left in the study. A monitoring visit takes place between your CRC and the CRO study monitor and can take all day. This will lead to your CRC’s time not being compensated every time the study monitor spends a day at your site. You should then re-negotiate the cost of your CRC spending all day with the CRO study monitor (recommended range between $500-$1,000) for each monitoring visit for the rest of the study).
In addition, the sponsor does not automatically budget for the time it takes for you and your study team to complete each new CRO’s policy training requirements (e.g. GCP training that you’ve already done that isn’t accepted by the CRO and you have to do it all over again, which can take hours- this needs to be budgeted). This time can be budgeted under the “administrative fees” cost mentioned in the first bullet point above.
As an aside, registry studies typically have high enrollment numbers with low payment per subject. The high enrollment rates in registries make up the low payment per subject, generally leading to coming out ahead in your budget.
If you have any questions regarding budgeting for your site, just contact the PRCSG Coordinating Center at prcsg@cchmc.org.
What is the difference between Local vs Central IRBs?
A local IRB (institutional review board) is an independent group that reviews proposals for research involving humans at hospitals within its jurisdiction. A central IRB is an IRB that conducts reviews on behalf of all study sites that agree to participate in the centralized review process. If you had the choice, which should you choose? PRCSG’s recommendation is to use a central IRB if you are allowed to do so by your institution, since you will save money and possibly shorten the time for IRB approval.
What is a CRO?
As a (prospective) site PI, you will engage with members from a CRO (e.g., Syneos, Iqvia). A CRO is a company hired by a pharmaceutical company to take over certain parts of running the clinical drug trial. For example, Pfizer hires Syneos to conduct the clinical trial; Pfizer still has a team, including a medical director, which oversees safety and efficacy, but Syneos conducts the day-to-day operation with the clinical site. For PRCSG supported trials, PRCSG Advisory Council Members often are on the Steering Committee and communicate with the Sponsor and the CRO in support of the site investigators.
What is a Monitoring Visit?
The CRO checks (monitors) to ensure that the clinical sites, supervised by the PIs, are following the protocol and that the trial is being conducted in compliance with regulatory requirements and ethical principles.
The PI and the CRC will engage directly with a CRO monitor. These CRO monitors often have high turnover during the study, especially when the study drags on for years. New CRO monitors to your site will take more of your time, so you need to account for this turnover in the budget (e.g., a large Children’s Hospital currently charges for CRO monitor turnover after the 2nd CRO monitor takes over).
What are the risks of participating in a trial that is not PRCSG supported?
- The clinical trial design may be a carbon copy of a previously conducted adult protocol and may not be pediatric friendly.
- The patients enrolled in the study may not receive access to trial medication once the experimental phase of the trial is complete.
- The protocol may not have been previously reviewed by PRCSG or a pediatric rheumatologist.
- You may not get publication opportunities as drug companies have their own authors, statisticians and medical directors that participate in the preparation of the manuscript.
What about post-trial drug access?
When participating in a clinical drug trial, the drug under investigation is typically a drug that you will not have access to outside of the trial. At the conclusion of the trial, if there is no provision in the protocol by the drug company to include free drug for a period of time after the trial, then the patient, who may have responded favorably to the investigational drug, will withdraw off the drug and possibly have a disease exacerbation. PRCSG only supports studies that provide free drug for a period after the study concludes.
Published references for free drug post-trial are available on PubMed and can be found on the PRCSG website (PMID 25878952, PMID 31759157). By taking part in a PRCSG trial, free drug post-trial can be included in the protocol. A potential downside of taking part in non-PRCSG industry trials is that some drug companies do not make provisions for free drug post-trial.
Sometimes, a CRO may approach a PI about a clinical trial.
PRCSG provides an umbrella of support for the conduct of multi-center pharmaceutical clinical trials in pediatric rheumatology. Early investigators may be approached separately by pharmaceutical companies and related entities to have their center participate in a clinical trial. It is advisable to be aware of the potential risks of engaging in these clinical trials without support from PRCSG.
Therefore, if you receive an email from someone you have never heard of that works for a drug company or CRO, inviting you to participate in a pediatric rheumatology clinical drug trial, please contact PRCSG (email is PRCSG@cchmc.org). This will help identify if the company has approached PRCSG about the trial, and if not, this alerts PRCSG about the existence of this trial.